What Causes Acid Reflux Disease?
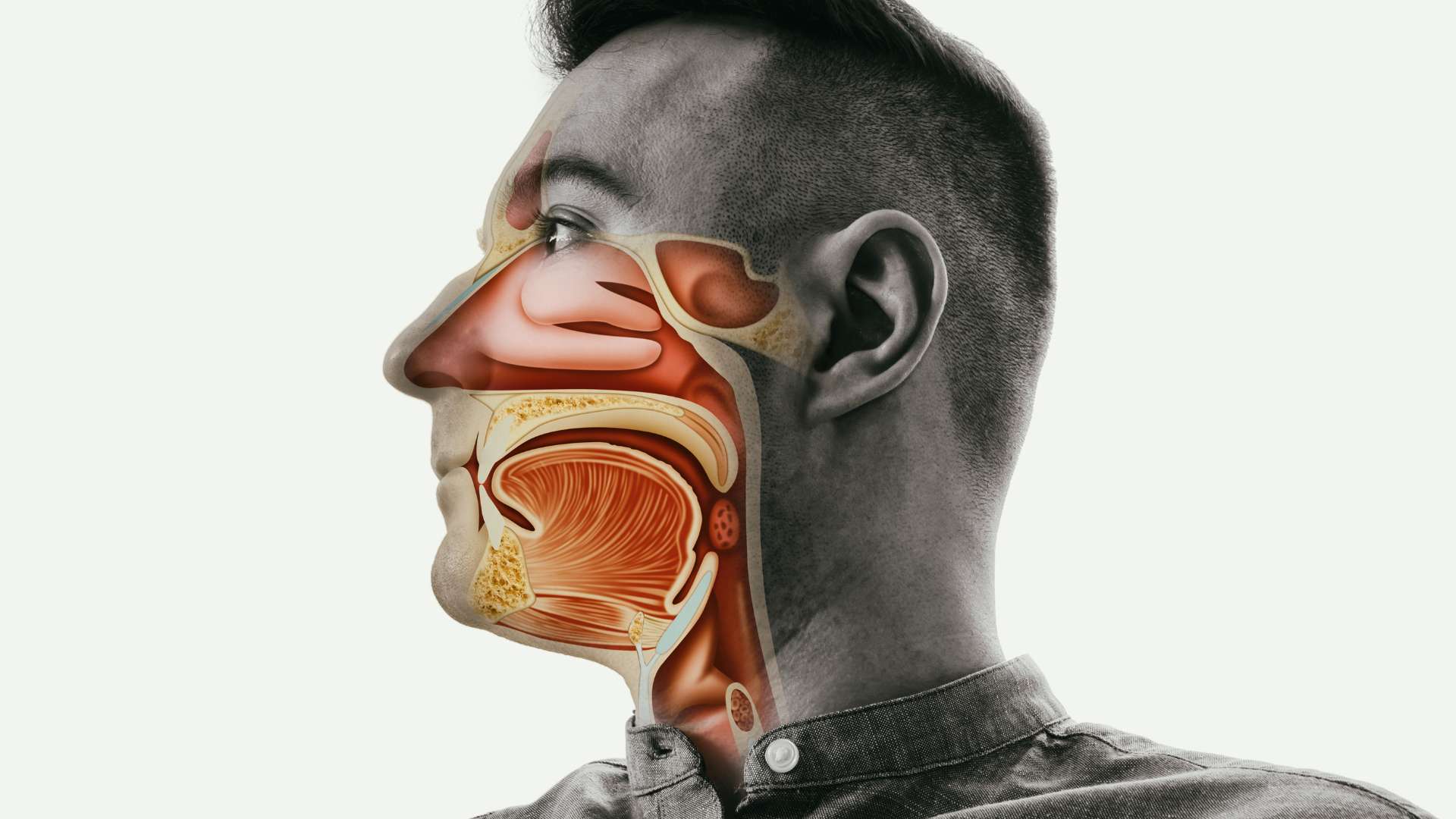
The underlying causes of acid reflux disease can vary, but one common factor is a stomach abnormality known as a hiatal hernia. This condition arises when the upper part of the stomach and the lower esophageal sphincter (LES) protrudes above the diaphragm, a muscular barrier that separates the stomach from the chest.
Typically, the diaphragm aids in keeping stomach acid where it belongs. However, in a hiatal hernia, acid can flow into the esophagus, leading to acid reflux disease symptoms.
Apart from hiatal hernias, several other risk factors contribute to the development of acid reflux disease:
Consuming large meals or reclining immediately after eating.
Being overweight or obese.
Eating substantial meals and lying flat on your back or bending at the waist.
Snacking close to bedtime.
Ingesting certain foods, such as citrus, tomatoes, chocolate, mint, garlic, onions, or spicy and fatty foods.
Drinking certain beverages, including alcohol, carbonated drinks, coffee, or tea.
Smoking tobacco products.
Pregnancy can also increase the likelihood of experiencing acid reflux.
Taking certain medications, such as aspirin, ibuprofen, specific muscle relaxers, or blood pressure medications.
Identifying and managing these risk factors can be crucial in alleviating or preventing acid reflux disease symptoms.
Acid Indigestion Symptoms
Common symptoms of acid indigestion include:
Heartburn: A burning sensation or discomfort that may migrate from the stomach to the abdomen, chest, or throat.
Regurgitation: The backing of sour or bitter-tasting acid into the throat or mouth.
Additional symptoms of acid reflux disease encompass:
Bloating
Passing bloody or black stools or experiencing bloody vomiting
Burping
Dysphagia: A feeling of food being stuck in the throat
Persistent hiccups
Nausea
Unexplained weight loss
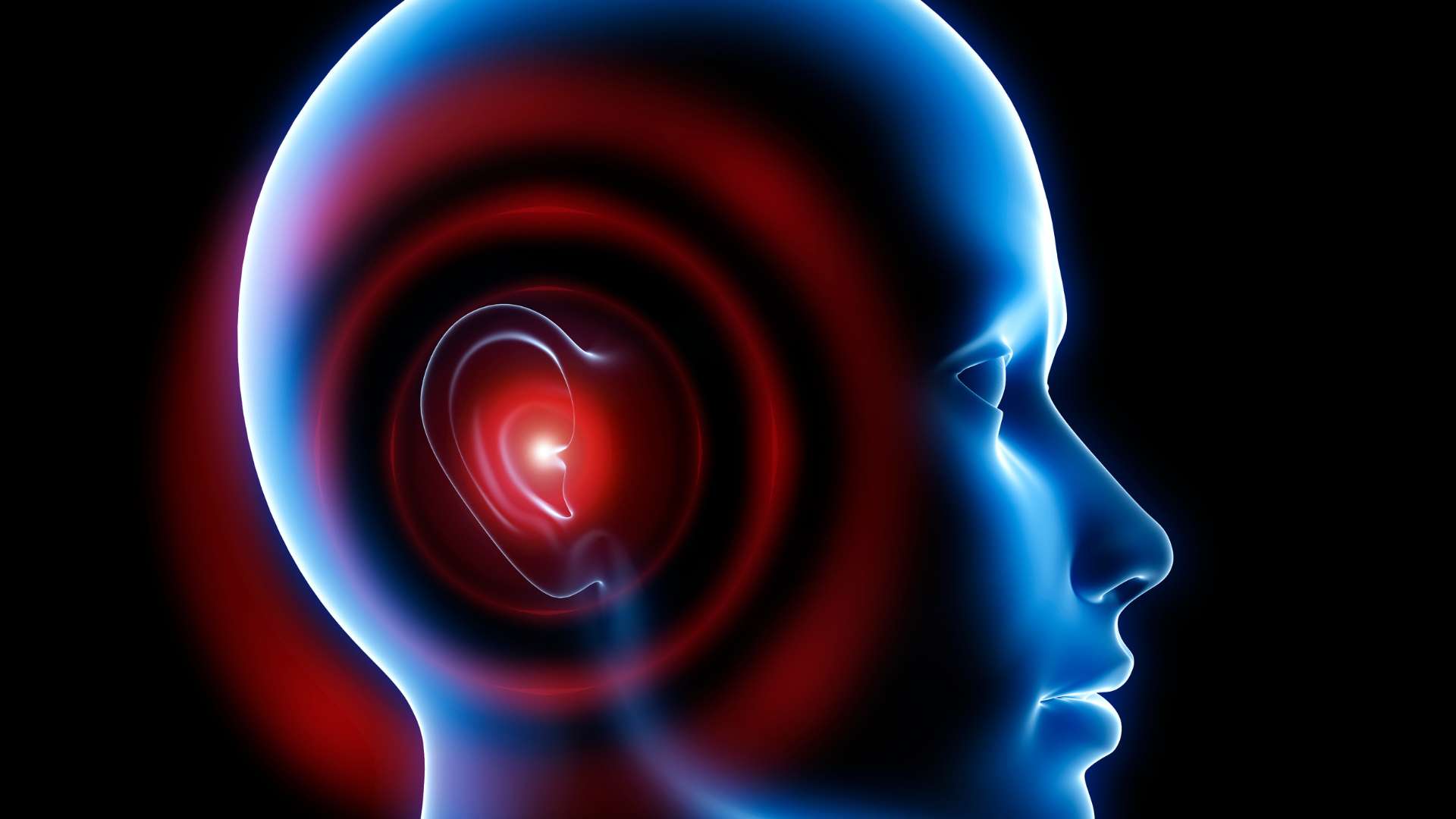
Wheezing, dry cough, hoarseness, or chronic sore throat
Bad breath and/or unpleasant taste in the mouth
Chest pain
Worsening of asthma symptoms.
How is Acid Reflux Disease Detected?
Medical attention is warranted to diagnose acid reflux disease if symptoms occur at least twice weekly or if relief from medications is insufficient. Key symptoms like heartburn aid in the diagnosis, along with lifestyle changes or acid-blocking medicines that alleviate the discomfort.
If symptoms persist or worsen, various tests can be conducted to confirm and assess potential complications. These tests include the barium swallow radiograph, endoscopy (EGD), biopsy, esophageal manometry, esophageal impedance monitoring, and pH monitoring.
These procedures help examine the esophagus, detect abnormalities, and measure acidity levels, providing valuable insights into the functioning of the esophageal sphincter.
How to Treat Acid Reflux Disease with Diet and Lifestyle Changes
A practical approach to managing acid reflux disease involves avoiding trigger foods and beverages. Alongside this, consider implementing the following measures:
Opt for smaller, more frequent meals and adjust your food choices.
Quit smoking.
Elevate the head of your bed by placing blocks, raising it by 4 to 6 inches.
Allow at least 2 to 3 hours between eating and lying down.
For daytime naps, try sleeping in a chair.
Avoid wearing tight clothing or belts.
If overweight or obese, pursue weight loss through exercise and dietary changes.
Consult your doctor about possible medication causing heartburn or other acid reflux symptoms.
Acid Reflux Disease Medications
A combination of lifestyle adjustments and over-the-counter medications is often sufficient to manage acid reflux disease symptoms. Antacids like Alka-Seltzer, Maalox, Mylanta, Rolaids, or Riopan can neutralize stomach acid, but overuse may lead to diarrhea or constipation.
It’s advisable to use antacids containing both magnesium hydroxide and aluminum hydroxide to counteract these gastrointestinal effects. If antacids prove ineffective, your doctor may explore other medications, some requiring a prescription.
They may recommend using a combination of medications, such as foaming agents (e.g., Gaviscon) to coat the stomach and prevent reflux, H2 blockers (e.g., Pepcid, Tagamet) to reduce acid production, proton pump inhibitors (e.g., Aciphex, Nexium, Prilosec, Prevacid, Protonix) to decrease stomach acid, or prokinetics (e.g., Reglan, Urecholine) to strengthen the LES, speed up stomach emptying, and alleviate acid reflux.
It’s crucial to avoid combining multiple types of antacids or medications without consulting your doctor first.
Has Acid Reflux Disease Ever Required Surgery?
Surgery may be recommended if medications fail to fully alleviate severe acid reflux disease symptoms and significantly impact your life. Two types of surgical treatments exist for GERD when daily medication use proves ineffective.
LINX Device: The most recent approved procedure involves placing a ring (LINX device) with magnetic titanium beads around the lower esophagus, preventing stomach contents from refluxing. Some patients in a study could reduce or stop medication usage. However, it’s unsuitable for those allergic to specific metals, and MRI tests are impossible with the LINX device.
Fundoplication: This surgery creates an artificial valve using the upper stomach to strengthen the LES, prevent acid reflux, and address hiatal hernias. Surgeons perform this through open cuts or minimally invasive techniques.
Surgery is a last-resort option when medical treatment fails to alleviate acid reflux disease effectively.